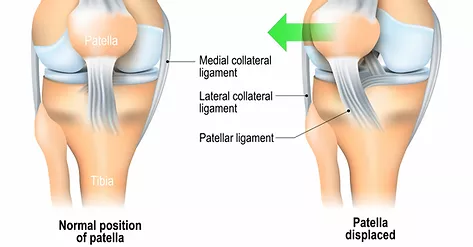
Patella dislocation is a common injury in adolescents, particularly in those playing sports. Most commonly, the patella dislocates laterally to the outside of the knee. This process often injures tissues on the medial or inside of the knee, such as the medial patellofemoral ligament (MPFL). Dislocation can be divided into two categories: primary (first-time) and secondary (second, third, etc). It may also be categorised as traumatic (involving significant force to dislocate the patella from its resting groove) or atraumatic.
The latter scenario can occur in individuals with ligament laxity. After the injury, an MRI is commonly performed to assess injury of bony and soft tissues of the knee cap, in order to guide management. These injuries have also been linked to osteoarthritis many years after the injury, and due to their high prevalence it is important to consider whether surgical or conservative management is best (Sanders et al. 2017).
Surgical vs Conservative Management
The ultimate aim in managing primary dislocations is to prevent another dislocation. A study published in 2017 found surgery to be superior to conservative management in the short-term, thus for professional athletes with return to sport pressure, this may be more suitable. However in the long-term, conservative and surgical management have the same outcomes in knee function when walking, squatting, climbing stairs and squatting (Longo et al. 2017)
Surgical Management
This being said, some injuries associated with patella dislocation may determine surgery necessary, such as osteochondral defect (which is an injury to the bone and cartilage of the knee cap), as it can increase rates of redislocation (Sanders et al. 2017). An orthopaedic specialist is often required to make this decision. The location of injury within the knee cap ligaments also may dictate if surgical management is necessary. (Kang et al. 2013)
Secondary (recurring) dislocations also require a specialist’s opinion, as this may indicate chronic instability of the patella due to injury of the supporting tissues. This does not mean surgery must be performed, as each patient’s individual anatomy affects the decision (Sanders et al. 2017).
Conservative Management
Conservative management principles have been debated within the literature. Firstly, duration of immobilisation post injury has varied from 2-6 weeks.
The commonly injured MPFL is maximally taught at 20-30 degrees of knee flexion, thus it is recommended to immobilise the leg straight in extension (Mistry et al. 2018). A ROM brace may be used, yet no studies to date have effectively assessed the best immobilisation method when comparing rates of redislocation.
Physiotherapy in the early stages often involves quadriceps activation exercises, weight bearing as tolerated, while the brace is on. VMO activation of the quadriceps is important due to its role in dynamically stabilising the patella and its relationship to the MPFL. (Desio et al. 1998) After a few weeks, the brace can be removed dependent on symptoms, and range of movement is gradually increased. A ROM brace is advantageous at this time to wean the flexion or bending range of movement.
As range improves, exercises may be progressed to incorporate further strength training of the pelvis and lower limb muscles. Proprioceptive training is also important to regain control of the knee, particularly in sports requiring change of direction and impact from external forces e.g. rugby.
Bracing can be helpful with those with symptoms of instability and apprehensiveness completing everyday tasks or even sports but it cannot prevent further dislocations. The brace usually involves a hole for the patella and a lateral buttress that provides support. (Brukner et al., 2017)
If you or someone you know have experienced a patella dislocation and would like physiotherapy rehabilitation, contact us at Xphysio for an assessment and treatment plan.
References
- Brukner, P., Khan, K., Clarsen, B., Cook, J., Cools, A., & Crossley, K. et al. (2017). Brukner & Khan’s clinical sports medicine (pp. 762-765). North Ryde, N.S.W.: McGraw-Hill Education (Australia).
- Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 1998;26(1):59–65.
- Kang, H. J., Wang, F., Chen, B. C., Zhang, Y. Z., & Ma, L. (2013). Non-surgical treatment for acute patellar dislocation with special emphasis on the MPFL injury patterns. Knee Surgery, Sports Traumatology, Arthroscopy, 21(2), 325-331.
- Longo, U. G., Berton, A., Salvatore, G., Migliorini, F., Ciuffreda, M., Nazarian, A., & Denaro, V. (2016). Medial patellofemoral ligament reconstruction combined with bony procedures for patellar instability: current indications, outcomes, and complications. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 32(7), 1421-1427.
- Mistry, J. B., Bonner, K. F., Gwam, C. U., Thomas, M., Etcheson, J. I., & Delanois, R. E. (2018). Management of injuries to the medial patellofemoral ligament: a review. The journal of knee surgery, 31(05), 439-447.
- Patellar Dislocation: Signs, Symptoms, Treatments | Total Orthopedics and Sports Medicine. (2017). Retrieved from https://www.totalorthosportsmed.com/patellar-dislocation-symptoms-treatments/
- Sanders, T. L., Pareek, A., Hewett, T. E., Stuart, M. J., Dahm, D. L., & Krych, A. J. (2018). High rate of recurrent patellar dislocation in skeletally immature patients: a long-term population-based study. Knee Surgery, Sports Traumatology, Arthroscopy, 26(4), 1037-1043.